PCR Testing: Is the “Gold Standard” Losing Some Luster?
By Emily Kim
Throughout this pandemic, PCR has been considered the “gold standard” of COVID-19 testing among the medical community. However, this test is still relatively new, and multiple sources point out its limitations.
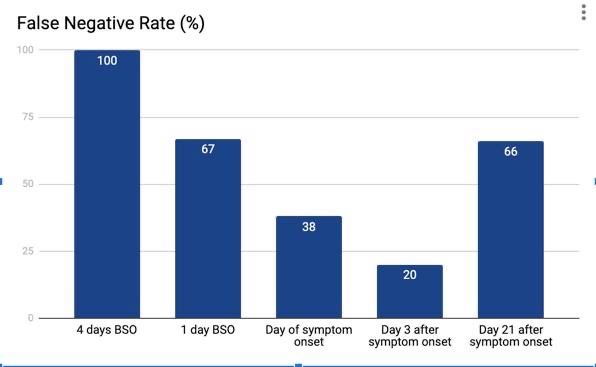
Researchers from the Annals of Internal Medicine synthesized data from seven different studies, in which 1330 individuals across all studies were administered PCR tests. The purpose of the study was to quantify the false negative rate by studying the number of days since infection. Though this research had its limitations, with the swabbing technique varying across all studies, it also had some notable findings.
Researchers found that between 0-4 days before symptom onset (BSO), the probability of a false negative decreased from 100% 4 days BSO to 67% 1 day BSO. On the day of symptom onset, the median false negative probability was 38%, reaching its lowest point 3 days AFTER symptom onset (day 8 in the study) at 20%. However, after this point, the probability of a false negative increased to 66% by day 21 after symptom onset.
These results cast doubt on the reliability of PCR as the “gold standard” of testing methods. Even one day prior to someone showing symptoms, the PCR test has a 67% probability of incorrectly diagnosing test subjects as negative for COVID-19. Furthermore, the study indicates that the longer someone waits to get tested after developing symptoms, the greater the likelihood is of getting a false negative result. Thus, at the conclusion of this study, researchers underscored how PCR tests should not be viewed as “end-all be-all” indicators of one’s health status. If people feel ill or doctors have a considerable amount of clinical suspicion that someone has COVID-19, they should take appropriate measures irrespective of the test result. Researchers also mentioned that using antibody testing along with PCR may be helpful in detecting COVID-19 in those “more remote from symptoms or exposure.”
Another study reported in a CNN article reinforces these findings. Dr. Michael Levin, professor of paediatrics and international child health at Imperial College London, treated children suffering from MIS-C—an inflammatory disease associated with COVID-19. Despite the children coming to Dr. Levin evidently ill, their PCR tests would come out negative for COVID-19. It was only after repeated PCR tests and even administering antibody tests that the children were identified as COVID-positive.
The same article also referenced Dr. James Schneider in New York, who faced a similar problem as Dr. Levin. He would test all of his MIS-C patients twice for COVID-19, because, as he stated at a CDC briefing, “PCR testing is not always accurate.”
What do we do with this information? There are two takeaways. First of all, the evidence seems to point to the fact that PCR tests alone may not be the most accurate in identifying COVID-positive patients. We should be open to the potential role of antibody testing in this process, and instead of choosing one over the other (PCR over antibody tests), see how they can work together. Secondly, it’s safe to say that people are eager to go back to “normal” life. People want to work, send their kids to school, go to school… and the aim of testing is to determine if people are healthy enough to do so. However, we can’t let the test results alone dictate our future actions. If your result comes out negative, then before you rush out to work, have your doctor assess your clinical state and overall well being. Test results, coupled with common sense, must guide our actions moving forward.